How to Get Rid of Bad Bacteria in the Gut

Gut dysbiosis is a condition where you have overgrowth of bad bacteria in the gut that can lead to annoying symptoms, leaky gut, and even whole body inflammation. In this article, you will learn how to cut the bad bacteria in the gut and heal with powerful medicinal herbs.
Before we dive into the herbs that can help cut the bugs in your gut, let’s first talk about what normal is and how it gets messed up.
Healthy Gut Microbiome
The healthy intestines of normal individuals are colonized by a wide range of bacteria of over 1,000 species and a total number of bacteria in the trillions.
The gut microbiome is the community of beneficial bacteria, fungi, yeast, and other microbes of over 1,000 species that live in our gut. The microbiome plays an essential role in health, as it affects metabolism, nutrient absorption, and immune function.
What Happens in a Healthy Gut
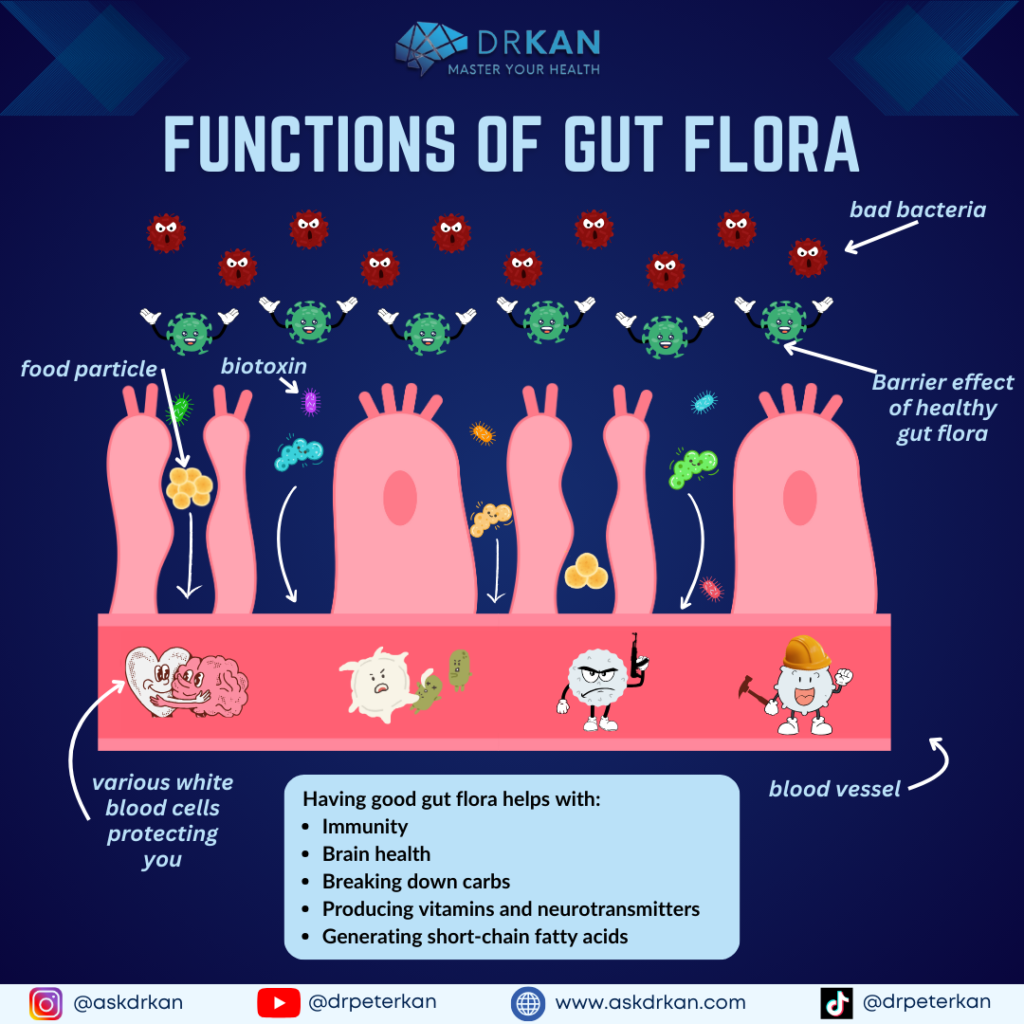
So, when you’re healthy, there’s this delicate balance between good and potentially bad bacteria in the gut. They’re like roommates in your intestines, and as long as everyone plays nice, everything runs smoothly. These bacteria aren’t just hanging out – they’re actually protecting you from getting sick by blocking out unwanted invaders. This protection is known as the “barrier effect,” or colonization resistance. Through the mucosal surface of the intestine, the microbiota interact with your immune system, providing you with immune regulatory functions, like priming the mucosal immune system.
The gut microbes also ferment foods, breaking down complex carbohydrates, making certain vitamins and neurotransmitters, and generating short-chain fatty acids, which you benefit from.
How a Healthy Gut Affects the Rest of Your Body
But wait, there’s more! Your gut buddies aren’t just confined to the gut – they’re influencers, reaching out and interacting with other organs like the brain.
This has led to studies of the influence of the gut microbiota on mental disorders, like autism, and diseases such as Alzheimer’s.
Aging, exposure to antibiotics, poor diet, and stress may potentially disrupt the microbial balance in the gut. Balance is the key for proper functioning in the gut microbiome in the GI system.
Dysbiosis (Too Many Bad Bacteria in the Gut)
When the gut microbes are out of balance, it’s called dysbiosis. Picture it as a party where the wrong guests show up and start causing trouble.
Dysbiosis is defined by an imbalance in bacterial composition, changes in bacterial metabolic activities, or changes in bacterial distribution within the gut.
There Are 3 Types of Dysbiosis
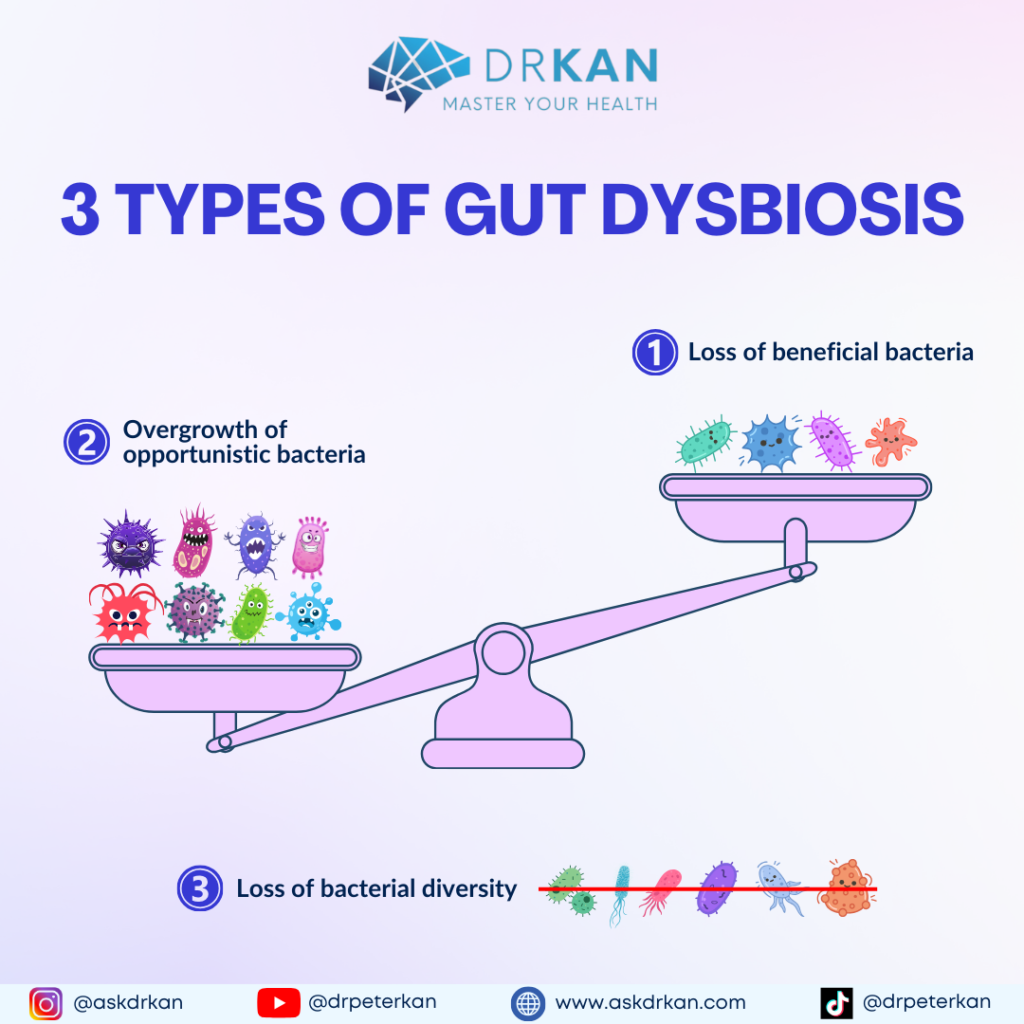
- Loss of beneficial bacteria
- Overgrowth of potentially pathogenic bacteria
- Loss of overall bacterial diversity.
In most cases, these 3 types of dysbiosis occur at the same time.
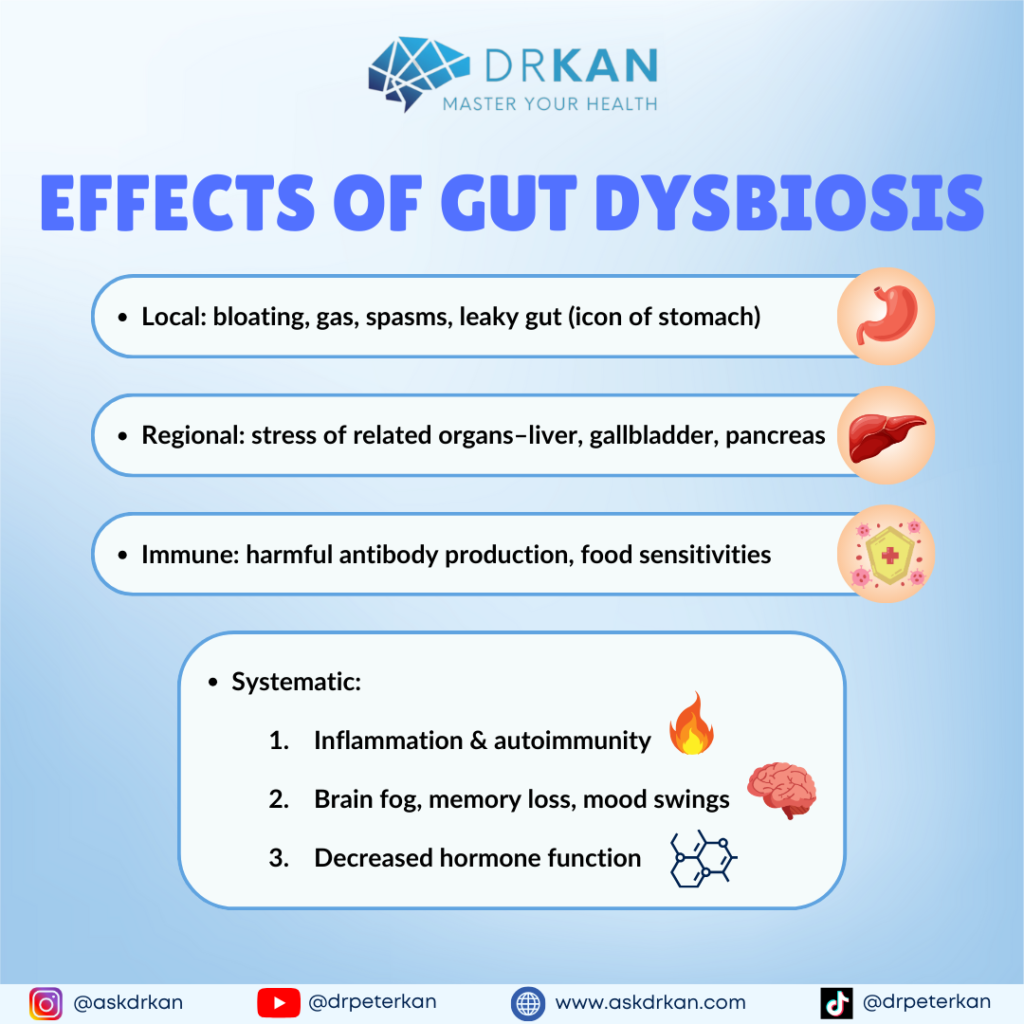
The effects of dysbiosis can go from local to systemic.
- Local: bloating, gas, spasms, inflammation, gut lining breakdown and leaky gut, malabsorption.
- Regional: stress or congestion of related digestive organs: liver, gallbladder, pancreas
- Immune: antibody production to partially digested food leading to food reactions
- Systemic:
- Aggravation of disorders in which inflammation is a key mechanism: migraines, arthritis, autoimmune disorders, etc.
- Central nervous system changes: brain fog, irritability, mood changes, anxiety, etc.
- Inflammation of hormone glands: leading to decreased hormone function
What Happens When You Have Too Many Bad Bacteria in the Gut?
A balanced and healthy gut microbiome can serve as a buffer to prevent infection and support your immune system. Changes in gut microbial composition and abundance can cause functional dysbiosis, making you more susceptible to pathogenic infections and development of diseases.
It’s important to know that all the microbes in the gut are all in competition for the finite amount of food, resources and real estate in the gut. When you have deficiency in the beneficial microbes, the bad bacteria in the gut overgrow.
When you have too much of a certain species of bacteria, it upsets the balance of power in the gut, and it changes immune response and the amount and types of bacterial metabolites that are produced. This change in the metabolites and immune response to the out of balance bacteria is primarily what is causing inflammation and disease.
Can You Have Too Many “Good” Bacteria?
This change occurs even if you have way too many beneficial microbes. We tend to think more is better. But when it comes to the gut microbiome, balance is the key. Too much of any type of microbe is dysbiosis and usually relates an inability of your immune system to control the microbes, or to an environment that feeds the microbes.
The environment that can feed the microbes can be a high refined carbohydrate diet, a diet full of sugar, chemicals and processed foods, environmental toxin exposure, stress, or other chronic inflammatory conditions, such as autoimmunity.
No matter the cause, dysbiosis always involves the overgrowth of certain microbes that are out of balance with other microbes in the gut.
Too Many Bad Bacteria in the Gut = Increased Inflammation
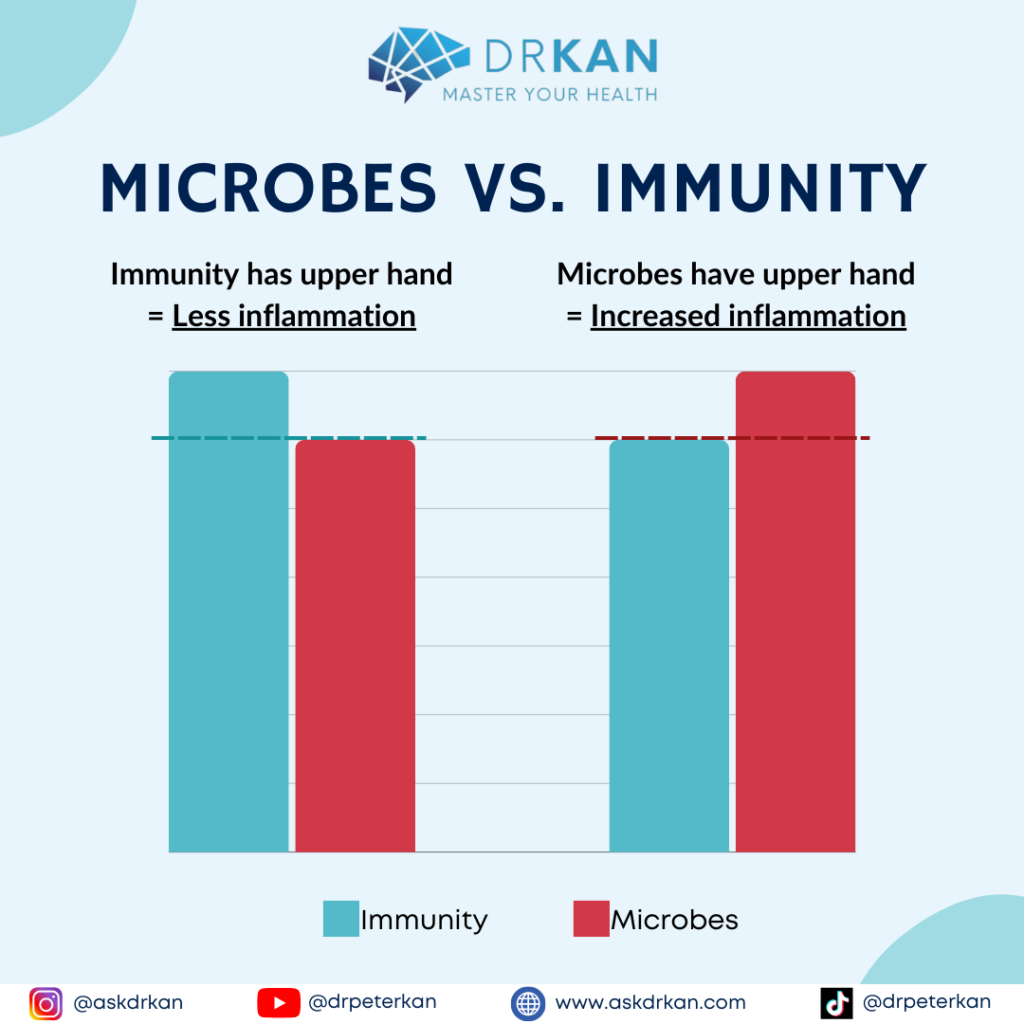
Carrying a high microbial load in the body is inherently inflammatory. This is because your immune system’s job is to control the amount of microbial load in the body, whether they are beneficial microbes or pathogenic ones.
And due to various reasons, such as chronic illness, chronic stress, and toxin overload, your immune system can become depleted, exhausted, or suppressed. This means that it cannot keep the overgrowth of microbes from becoming out of control.
This is where outside help with compounds that can help reduce microbial load can give your immune system a break, reduce pathogen load, restore gut microbial imbalance, heal the gut, reduce inflammation, and potentially reverse a whole host of symptoms as a result of the brain-immune-gut axis dysfunction.
Should You Use Antibiotics to Remove Bad Bugs in the Gut?
When you have an imbalance of microbes in the gut, your immune system may need help. The outside help can be with antibiotic medications. But using antibiotics is akin to dropping the nuclear bomb on the gut microbiome! It’s indiscriminately wiping out all the microbes, good or bad. And this may have dire consequences and side effects. It has its time and place, but not every time and every place.
That’s where natural herbs come in. They are not as decisive in their action as antibiotics, so they are not a replacement for antibiotic medications if you need it for an acute medical condition.
And that is also the reason the herbs don’t carry the side effect profile of medications. The antimicrobial herbs tend to be more discriminant in how it goes about trimming the microbes. They tend to have more activity against pathogenic microbes and less activity on the beneficial microbes. In addition to antimicrobial properties, many of these herbs also have anti-inflammatory and metabolic effects that are beneficial as well, making them holistic superstars.
Herbs That May Have an Antimicrobial Effect in the Gut
Here are herbal compounds that can help with dysbiosis to restore a balanced gut microbiome.
Tribulus terrestris
Tribulus Extract has been used medicinally in traditional Chinese and Indian medicines for centuries.
It contains many bioactive compounds including saponins and alkaloids that may have health‑promoting properties, such as the support of GI microbial balance. It also helps support testosterone and adrenal function.(1)
Tribulus has been shown to exhibit antibacterial activity against several types of pathogenic bacteria and yeast, including Enterococcus faecalis, Staphylococcus aureus, Escherichia coli, Candida albicans, certain strains of Salmonella, Proteus vulgaris, Cornybacteria diphtheriae, and Pseudomonas aeruginosa.(1)
Berberine Sulfate (Berberis aristata)
Berberine is a bitter‑tasting, yellow plant alkaloid found in the roots, rhizomes, and stem bark of various plants, including Oregon grape, barberry, and goldenseal. Berberine has been shown to have antimicrobial, antiviral, and anti‑parasitic properties, including properties against potential pathogens in the GI microbiome.(2,3,4)
It has been shown to inhibit the growth of Giardia lamblia, Vibrio cholera, and Entamoeba histolytica. Studies have also demonstrated its potential to inhibit yeast and several species of bacteria, including C. albicans, S. aureus, E. coli, and P. aeruginosa.(5)
A systematic review and meta‑analysis reviewed 13 randomized controlled trials that added berberine in doses ranging from 120 mg to 500 mg to standard triple therapy treatment for 1 to 2 weeks for Helicobacter pylori eradication. The researchers found that the addition of berberine significantly improved H. pylori eradication rates. It also increased the healing rate of peptic ulcers, supported the relief of clinical symptoms, and reduced the incidence of adverse events compared to standard therapy.(2)
Studies have also demonstrated the potential for berberine to be effective against Clostridium difficile, including as an adjunct therapy alongside vancomycin, helping to prevent a relapse infection of C. difficile.(6)
Berberine may support GI health by strengthening intestinal tight junctions and reducing gut permeability, an effect observed in human intestinal epithelial cells in vitro.(7)
On top of the GI supportive effects, berberine has been shown to support healthy blood glucose levels, as well as supporting TH1 innate immunity. (8)
Artemisinin
Artemisinin is derived from the inner bark of the Artemisia annua tree. Its common name was dubbed “wormwood,” owing to its noted ability to kill parasitic worms. This compound has long been used as an antimalarial.(9)
Studies have demonstrated its efficacy against parasites that induce GI symptoms and various pathogenic bacteria and fungi, including S. aureus, Staphylococcus epidermidis, Enterobacter faecalis, Enterobacter cloacae, E. coli, S. typhimurium, and C. albicans.
It has also been shown to be effective against a range of viruses, including human cytomegalovirus, Epstein‑Barr virus, herpes simplex type 1, and hepatitis B and C.(10,11)
Artemisinin also supports antioxidant status and immune function. (10)
Black Walnut Extract
Black Walnut Extract has a long history of use as an intestinal antiparasitic (vermifuge, anthelmintic) in botanical medicine. It also possesses activity against common bacterial and fungal pathogens that occur in GI dysbiosis. There have been at least six distinct bioactive compounds with antibacterial effects identified in black walnuts, some of which are also antiviral, antifungal, and antiparasitic/antiprotozoal.(12)
Black walnut extract has been shown to be effective against S. aureus. Black walnut extract also has potent anti‑inflammatory effects and was shown to inhibit secretion of several inflammatory cytokines in cultured human promonocytes.(13)
Uva Ursi
Bearberry Extract, also called uva ursi, has been used as medicine dating back to the 13th century. Uva‑ursi contains a compound called arbutoside, which is converted in the gut and liver to hydroquinone. Hydroquinone has antiseptic effects in the GI and urinary tracts. (14)
Uva‑ursi has been shown to have antibacterial action against pathogenic organisms including P. aeruginosa.(14)
Caprylic Acid
Caprylic acid is a medium‑chain fatty acid found naturally in coconut and palm kernel oils and breast milk. Due to its relatively short chain length, caprylic acid is able to penetrate and disrupt bacterial cell membranes and reduce biofilm formation. (15)
It has been shown to be effective against inhibiting the growth of C. difficile. (15) It has also been found effective against inhibiting C. albicans and its biofilm formation.(16)
My Favorite Way to Correct Dysbiosis (Bad Bacteria in the Gut)
Each of these herbs can powerfully help to restore your gut microbial balance. Imagine if you stack them and use them all together. You will get a synergistic effect that is greater than using them individually.
This is why I use GI Detox Pro in my practice to support the gut microbiome when there is dysbiosis.

GI Detox Pro is a targeted blend of nutrients and botanicals with a long history of use for supporting a healthy microbial balance within the GI tract.
This proprietary blend of botanicals includes Tribulus extract, berberine, bearberry extract, black walnut powder, barberry extract, artemisinin, along with magnesium and caprylic acid from magnesium caprylate.
Research shows that the bioactive constituents in these botanicals possess properties that may help promote a healthy balance of normal gut flora.
The ingredients in GI Detox Pro work synergistically to help support a normal balance in the gut microbiome.
Each 1‑capsule serving contains:
- 200 mg of Tribulus extract standardized to contain 40% saponins to support GI microbial balance
- 100 mg of berberine sulfate and 50 mg of barberry extract standardized to contain 6% berberine to support gut health
- 150 mg of magnesium caprylate, yielding 120 mg caprylic acid to support the disruption of bacteria cell formations and biofilm synthesis
- 100 mg of bearberry extract standardized to contain 20% arbutin
- 100 mg of black walnut powder, and 15 mg of artemisinin to help support the body’s immune responses
Benefits:
- Supports GI microbial balance
- Supports the body’s immune responses
- Supports immune health in the GI tract
- Supports gut health
This product can be supportive for those with dysbiosis, SIBO, H pylori, candida overgrowth, parasites, and UTI.
How to Use GI Detox Pro to Help Correct Dysbiosis
- General recommended use: For therapeutic effect, I recommend 2 capsules twice per day on an empty stomach. (Taking GI Detox Pro on an empty stomach may have more biofilm disrupting effect.)
- If you are sensitive, you may start with 1 cap per day and work your way up to the therapeutic dosage. You may also take the supplement with food if you tend to be sensitive to supplements.
- How long to take it: Minimum for 4 weeks. You can take it for 3-6 months for chronic dysbiosis and reassess to see how you are doing and if additional rounds are necessary.
For more complex cases, I normally recommend using GI Detox Pro along with the following supplements:
- If you suspect leaky gut, which usually accompanies gut dysbiosis, GI Resuscitate can be used at the same time.
- If you are looking to bolster the gut microbiome as you are cutting the bugs in your gut, consider adding Symbiome Plus, which is a full spectrum probiotic with bacteriophage which serves as a prebiotic as well as having selective antimicrobial effects.
Want More Individualized Help?
We offer Zoom consultations to help you identify the root cause. We order functional medicine lab tests for you and design a customized eating plan, supplementation plan and detoxification plan to optimize health while reducing the dependency on medications.
If your struggling with chronic symptoms, and looking for root cause approach using a natural and holistic approach, please visit https://askdrkan.com/get-started for more information and to get started on the path to wellness.
References
- Chhatre S, Nesari T, Somani G, Kanchan D, Sathaye S. Phytopharmacological overview of Tribulus terrestris. Pharmacogn Rev. 2014;8(15):45–51. doi:10.4103/0973‑7847.125530.
- Hu Q, Peng Z, Li L, et al. the efficacy of berberine‑containing quadruple therapy on helicobacter pylori eradication in China: a systematic review and meta‑analysis of randomized clinical trials. Front Pharmacol. 2020;10:1694.
- Imanshahidi M, Hosseinzadeh H. Pharmacological and therapeutic effects of Berberis vulgaris and its active constituent, berberine. Phytother Res. 2008;22(8):999–1012. doi:10.1002/ptr.2399.
- Imenshahidi M, Hosseinzadeh H. Berberis vulgaris and berberine: an update review. Phytother Res. 2016;30(11):1745– 1764.
- Pandey G, Khatoon S, Pandey MM, Rawat AKS. Altitudinal variation of berberine, total phenolics and flavonoid content in Thalictrum foliolosum and their correlation with antimicrobial and antioxidant activities. J Ayurveda Integr Med. 2018;9(3):169–176.
- Wultańska D, Piotrowski M, Pituch H. The effect of berberine chloride and/or its combination with vancomycin on the growth, biofilm formation, and motility of Clostridioides difficile. Eur J Clin Microbiol Infect Dis. 2020;39(7):1391‑1399. doi:10.1007/s10096‑020‑03857‑0
- Gu L, Li N, Li Q, et al. The effect of berberine in vitro on tight junctions in human Caco‑2 intestinal epithelial cells. Fitoterapia. 2009;80(4):241–248. doi:10.1016/j.fitote.2009.02.005.
- Kim TS, Kang BY, Cho D, Kim SH. Induction of interleukin-12 production in mouse macrophages by berberine, a benzodioxoloquinolizine alkaloid, deviates CD4+ T cells from a Th2 to a Th1 response. Immunology. 2003 Jul;109(3):407-14.
- Ho WE, Peh HY, Chan TK, Wong WS. Artemisinins: pharmacological actions beyond anti‑malarial. Pharmacol Ther. 2014;142(1):126–139. doi:10.1016/j.pharmthera.2013.12.001
- Abiri R, Silva ALM, de Mesquita LSS, et al. Towards a better understanding of Artemisia vulgaris: botany, phytochemistry, pharmacological and biotechnological potential. Food Res Int. 2018;109:403–415. doi:10.1016/j.foodres.2018.03.072
- Pandey N, Pandey‑Rai S. Updates on artemisinin: an insight to mode of actions and strategies for enhanced global production. Protoplasma. 2016;253(1):15–30. doi:10.1007/s00709‑015‑0805‑6
- Ho KV, Lei Z, Sumner LW, et al. Identifying antibacterial compounds in black walnuts (Juglans nigra) using a metabolomics approach. Metabolites. 2018;8(4):58. doi:10.3390/metabo8040058.
- Ho KV, Schreiber KL, Vu DC, et al. black walnut (Juglans nigra) extracts inhibit proinflammatory cytokine production from lipopolysaccharide‑stimulated human promonocytic cell line U‑937. Front Pharmacol. 2019;10:1059. doi:10.3389/ fphar.2019.01059.
- Tolmacheva AA, Rogozhin EA, Deryabin DG. Antibacterial and quorum sensing regulatory activities of some traditional Eastern‑European medicinal plants. Acta Pharm. 2014;64(2):173–186. doi:10.2478/acph‑2014‑0019.
- Kim HW, Rhee MS. Response surface modeling of reductions in uropathogenic Escherichia coli biofilms on silicone by cranberry extract, caprylic acid, and thymol. Biofouling. 2018;34(6):710–717.
- Lee JH, Kim YG, Khadke SK, Lee J. Antibiofilm and antifungal activities of medium‑chain fatty acids against Candida albicans via mimicking of the quorum‑sensing molecule farnesol. Microb Biotechnol. 2021;14(4):1353‑1366.