The Vital Link Between Blood Sugar Imbalance and Chronic Inflammation: A Comprehensive Guide

If you’re struggling with chronic inflammation or autoimmune conditions, you may already be familiar with anti-inflammatory medications and supplements. However, a less often discussed but crucial factor could be blood sugar imbalances.
Blood sugar imbalance, whether it’s low or high, can fuel inflammation and intensify symptoms in autoimmune disorders.
Stabilizing blood sugar may significantly enhance your ability to manage inflammation and support overall health.
How Blood Sugar Imbalance Affects More Than Just Metabolism
Blood sugar imbalances aren’t limited to metabolic issues like weight gain or mood swings. They also affect brain health, digestive function, and even the immune system. This contributes to a cycle of inflammation and neurodegenerative risk.
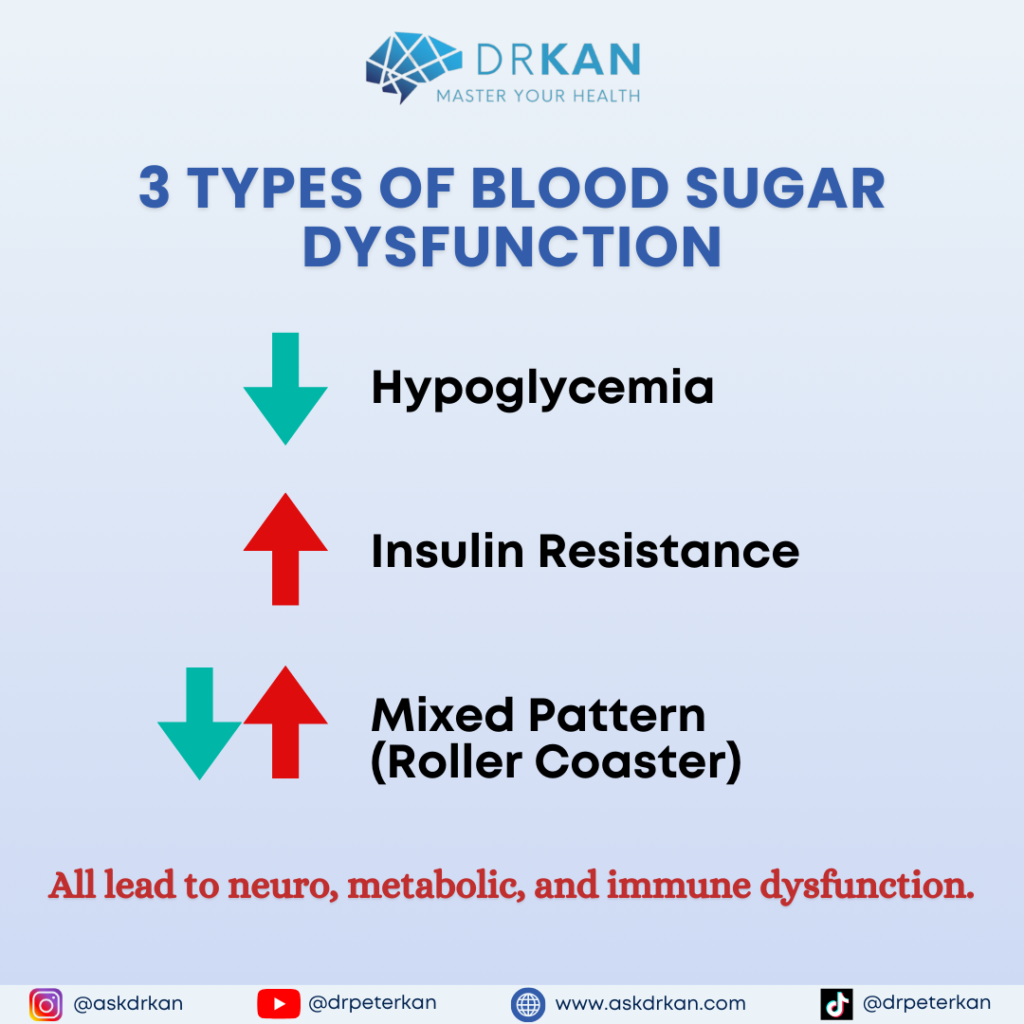
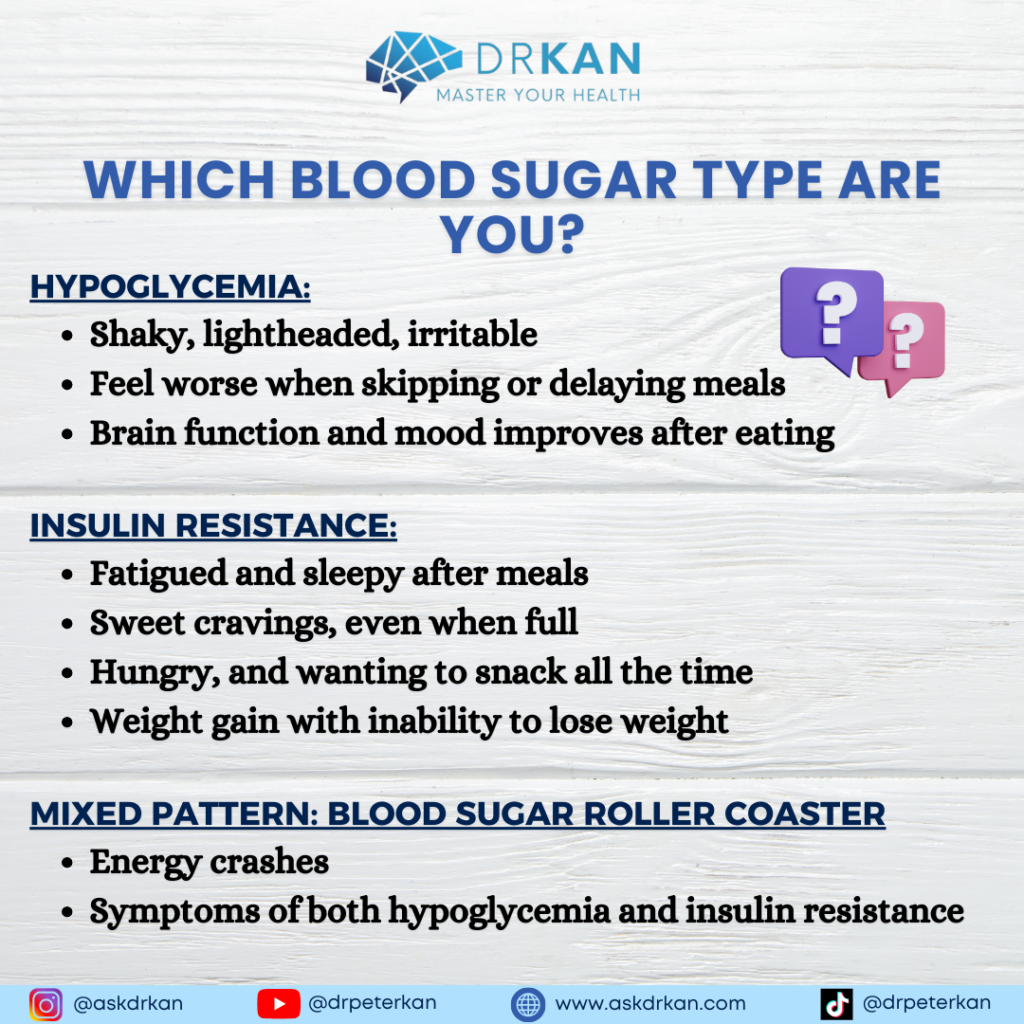
Blood sugar dysfunction comes in 3 flavors:
- Hypoglycemia (low blood sugar)
- Hyperglycemia (high blood sugar)
- Mixed pattern (both high and low blood sugar)
All three types are tied to different symptoms and outcomes. But the end results all lead to inflammation and eventual metabolic dysfunction and neurodegeneration.
Type 1: Low Blood Sugar: Reactive Hypoglycemia and Its Impact on the Brain and Body
Reactive hypoglycemia is a temporary drop in blood sugar levels following a high-carbohydrate meal. This can disrupt brain function and drive inflammatory responses throughout the body.
What Causes Reactive Hypoglycemia?
Reactive hypoglycemia occurs when you consume sugary or carb-heavy foods, leading to a spike in blood sugar levels. As your body releases insulin to bring down your blood glucose, levels can drop drastically, resulting in a hypoglycemic episode. This fluctuation can significantly impact cognitive and physical health, especially in those sensitive to these swings.
Effects on Brain Function and Mental Clarity
The brain is particularly sensitive to blood glucose fluctuations. When blood sugar drops:
- Cognitive Function Declines: With low glucose, brain cells fire less frequently, leading to slowed mental processing.
- Symptoms of Brain Fog and Fatigue: Common signs include brain fog, reduced memory, lack of motivation, and even depression.
Vagus Nerve Dysfunction and Digestive Health
The vagus nerve, responsible for connecting the brain to the digestive system, is also impacted by low blood sugar. Reduced vagal tone can lead to:
- Poor digestion: Symptoms such as constipation, bloating, and even leaky gut.
- Increased Inflammatory Response: The vagus nerve plays a role in modulating inflammation, so low blood sugar may contribute to higher baseline inflammation.
Type 2: High Blood Sugar and Insulin Resistance: How They Drive Chronic Inflammation
High blood sugar levels can lead to insulin resistance, a state where cells no longer respond effectively to insulin. This condition is a significant driver of inflammation and can spiral into type 2 diabetes if not managed.
Understanding Insulin Resistance and Its Role in Inflammation
When blood sugar imbalances result in levels that are consistently high, the body responds by releasing more insulin to manage glucose levels. However, chronic exposure to elevated insulin causes cells to become resistant. This condition leads to:
- Increased Blood Sugar: Unresponsive cells result in higher glucose levels in the bloodstream.
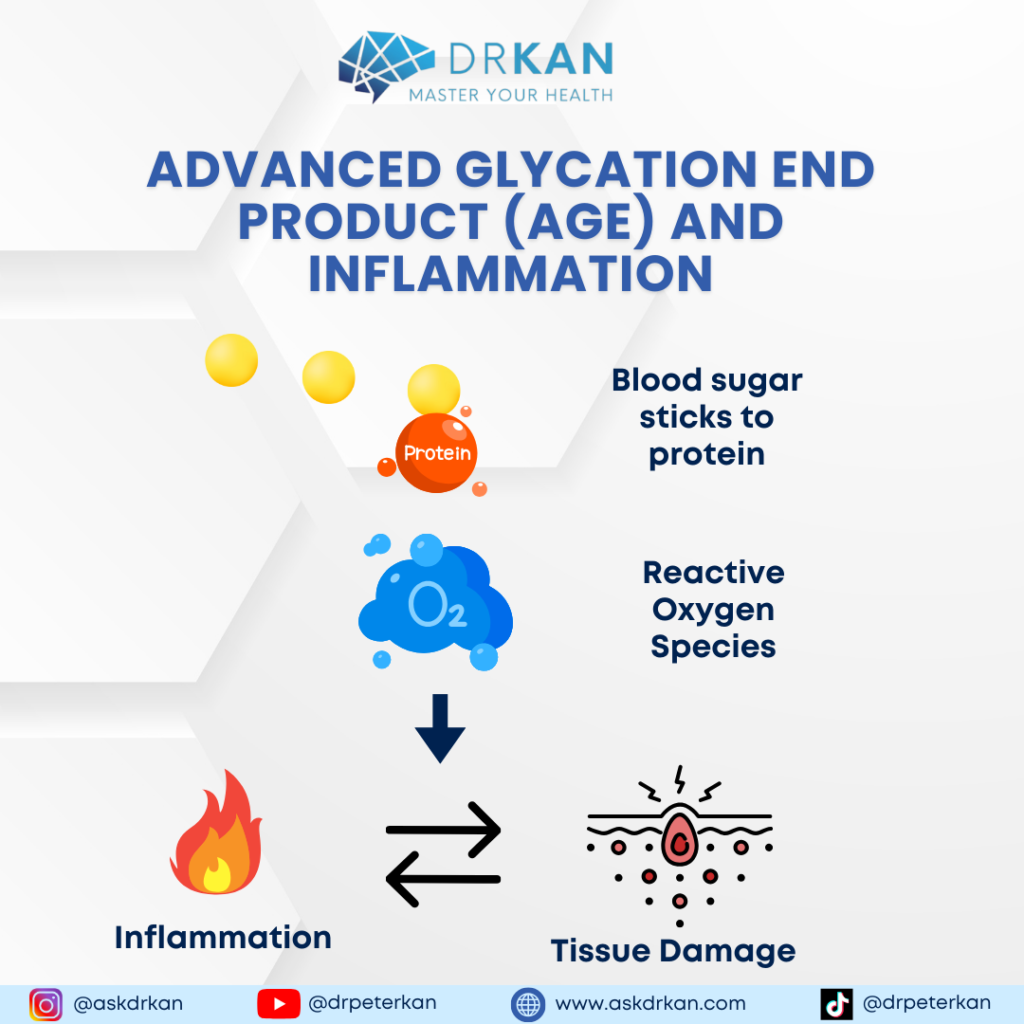
- Inflammatory Markers: Elevated blood sugar causes Advanced Glycation End Products (AGEs) to form, creating oxidative stress and cellular damage.
Advanced Glycation End Products (AGEs) and Their Inflammatory Impact
AGEs result when sugars bind to proteins, making cells “sticky.” This “caramelization” of cells is extremely inflammatory and prompts the immune system to react as if it’s facing a threat. Increased AGEs:
- Trigger immune responses through Damage-Associated Molecular Patterns (DAMPs).
- Drive up chronic inflammation, contributing to autoimmune disease flare-ups and tissue degradation.
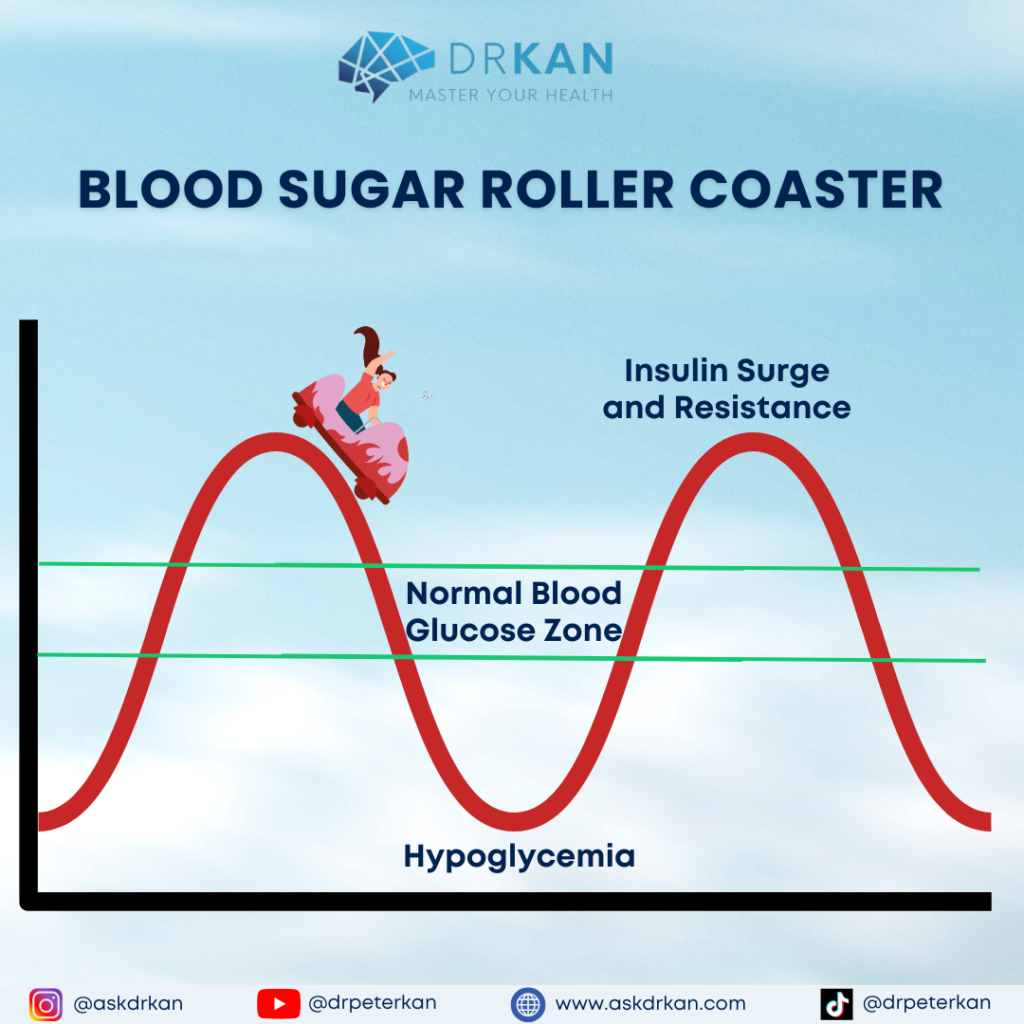
Type 3: Mixed Pattern: Blood Sugar Roller Coaster
You may have both low and high blood sugar problems. Normally, your blood sugar level will fluctuate within a normal range. A mixed blood sugar pattern means that your blood sugar level rises and falls like a roller coaster, much more than the normal fluctuations that accompany a healthy metabolism.
Excessive blood sugar swings can lead to energy crashes, mood swings, and cognitive dysfunction.
This wild blood sugar swing causes you to experience the lows of hypoglycemia part of the time. At other times, your blood sugar imbalances lead to insulin surges that cause insulin resistance, metabolic syndrome, and inflammation.
How Lifestyle Choices Fuel Blood Sugar Imbalance
Your diet, exercise routine, and even caffeine habits can greatly affect blood sugar levels. Making informed choices in these areas can be essential for achieving a more stable blood sugar pattern and reducing inflammation.
Diet Choices Leading to Hypoglycemia
Skipping meals or eating processed, carb-heavy snacks may contribute to blood sugar crashes. Here’s how:
- Skipping Breakfast: Leads to lower blood glucose throughout the day.
- Relying on Sugary Snacks: Provides temporary energy spikes, followed by rapid crashes.
- Excessive Caffeine: When used as a substitute for meals, caffeine can suppress appetite and mask signs of hypoglycemia, exacerbating adrenal stress.
Factors Contributing to Insulin Resistance
For those struggling with insulin resistance, lifestyle factors like overeating, high-carb diets, and low physical activity are common contributors:
- High-Carbohydrate, Low-Fiber Diets: Fiber helps regulate glucose entry into the bloodstream, and low fiber intake can accelerate insulin resistance.
- Sedentary Behavior: Lack of physical activity reduces the body’s ability to clear glucose, leading to high blood sugar accumulation.

Recognizing the Symptoms of Blood Sugar Imbalance
Being aware of your body’s signals can help you identify whether you’re experiencing hypoglycemia or insulin resistance.
Type 1: Hypoglycemia Symptoms
Those with low blood sugar may feel:
- Shaky and lightheaded: Especially after skipping meals.
- Feeling better after eating: Brain function and mood improves after meals.
- Irritable and anxious: A condition often referred to as feeling “hangry.”
- Brain fog and blurry vision: Reflecting the brain’s glucose deficiency.
Type 2: Insulin Resistance Symptoms
Those with high blood sugar may experience:
- Fatigue after meals: A sign that glucose is not effectively entering cells
- Intense cravings for sweets: Often after meals, as the body’s cells signal for more energy
- Persistent hunger and weight gain: Insulin resistance reduces satiety signals, leading to overeating.
Type 3: Mixed Pattern Blood Sugar Roller Coaster Symptoms
- Feeling lightheaded, shaky, irritable when meals are skipped or delayed
- Fatigue and sleepiness after meals
- Carb and caffeine cravings
- Energy crashing throughout the day
Long-Term Health Risks Associated with Blood Sugar Imbalance
When left unaddressed, both hypoglycemia and insulin resistance can lead to chronic health conditions.
Conditions Linked to Hypoglycemia
Low blood sugar may contribute to:
- Chronic fatigue and mood disorders: Conditions like anxiety and depression
- Hormonal imbalances: Blood sugar instability can disrupt hormones involved in regulating energy, like cortisol and adrenaline.
Conditions Linked to Insulin Resistance
Persistent high blood sugar can cause:
- Obesity and difficulty losing weight: Excess glucose is stored as fat.
- Cardiovascular issues: The inflammatory nature of insulin resistance increases heart disease risk.
- Hormone disorders: Conditions like polycystic ovarian syndrome (PCOS) in women and low testosterone in men.
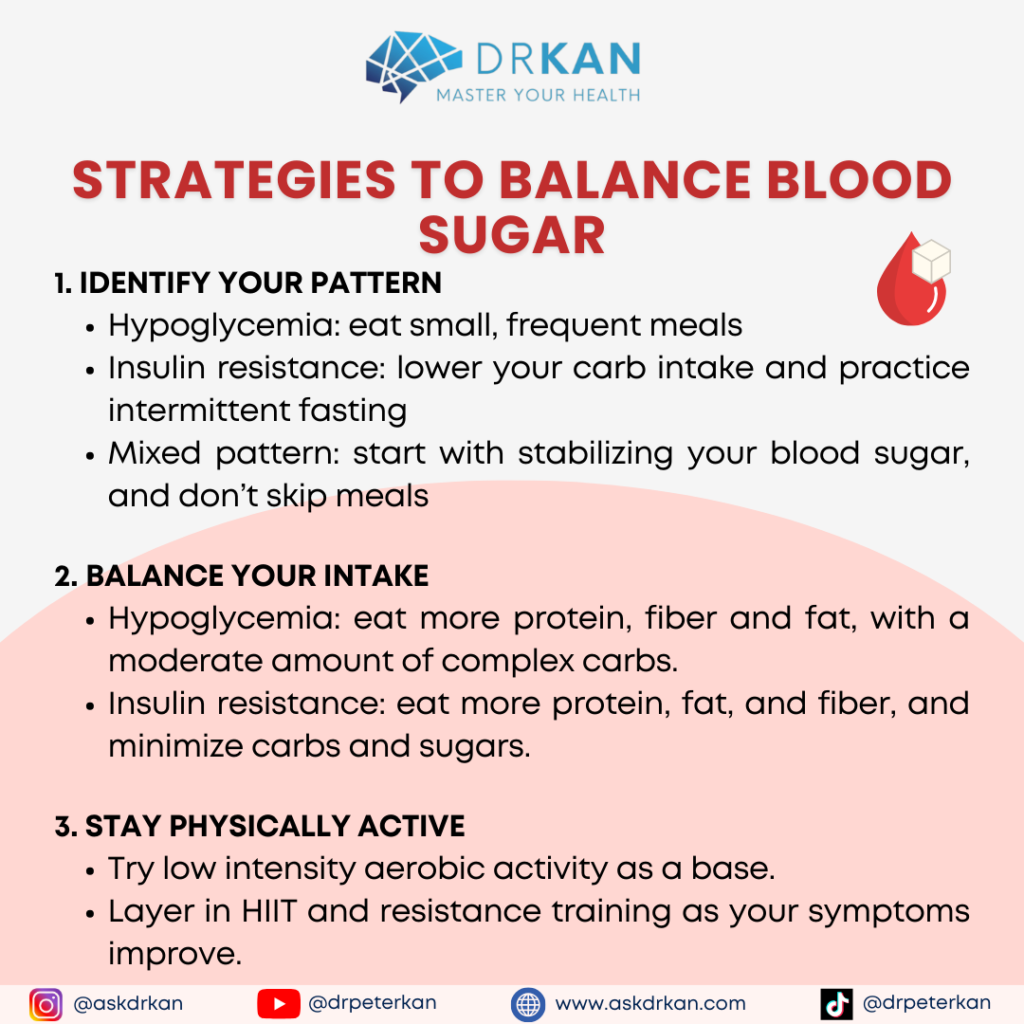
Strategies to Balance Blood Sugar and Reduce Inflammation
For those managing chronic inflammation or autoimmunity, blood sugar stabilization should be a priority. Here’s how you can start:
Step 1: Identify Your Blood Sugar Pattern
The first step is recognizing your blood sugar pattern:
- Hypoglycemia: You may feel shaky and lightheaded when you skip meals and feel better after eating.
- Insulin Resistance: You may often be fatigued after meals, struggle with cravings, and find it difficult to lose weight.
Step 2: Make Lifestyle Adjustments for Blood Sugar Control
By making conscious choices around diet, exercise, and meal timing, you can manage blood sugar imbalances and support inflammation control.
Focus on Balanced Meals
Ensure that meals contain a balance of healthy fats, proteins, and fiber to avoid blood sugar spikes. Examples include:
- Wild-caught fish and leafy greens: These are good sources of omega-3s and antioxidants.
- Complex carbs: Whole grains (as tolerated) and legumes are good for sustained energy.
Regular Physical Activity
Exercise is one of the quickest ways to lower blood sugar. It promotes glucose uptake into muscle cells, reducing insulin resistance over time. Aim for a combination of aerobic and resistance training for optimal results.
Step 3: Minimize Sugar and Processed Foods
Refined sugars and carbohydrates have immediate and pronounced effects on blood glucose. Replace them with:
- Fiber-rich alternatives like fresh fruits and vegetables.
- Whole grains and legumes that release glucose more gradually.
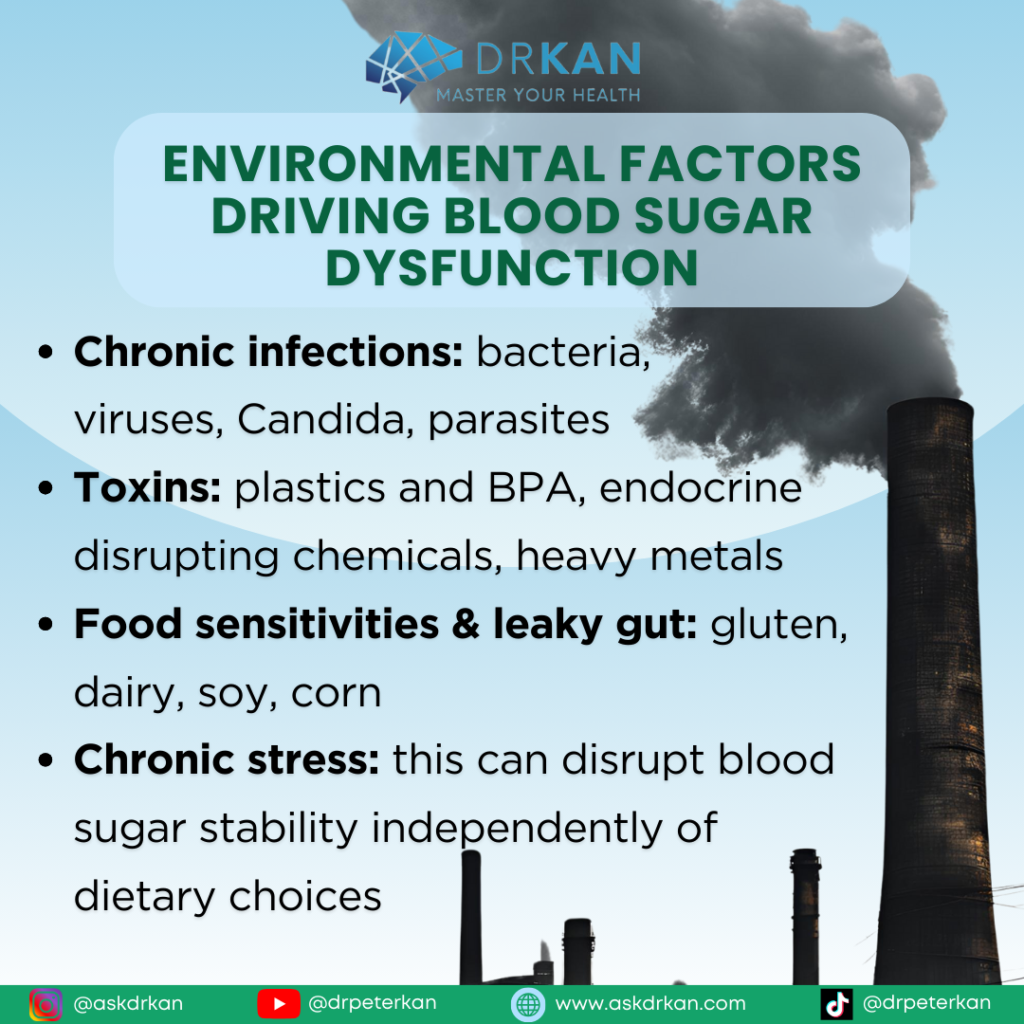
Advanced Approaches to Stabilize Blood Sugar Imbalance and Control Inflammation
Blood sugar dysregulation can sometimes be driven by neurometabolic imbalances or environmental factors, requiring more comprehensive solutions.
Neurometabolic Factors and Inflammation
Chronic infections, toxin exposure, and even food sensitivities can cause a persistent inflammatory state, complicating blood sugar control:
- Infections: Chronic infections (like Candida or parasites) can disrupt blood sugar balance and promote inflammation.
- Toxins: Exposure to environmental toxins such as plastics or heavy metals can interfere with metabolic function.
- Food sensitivities and leaky gut: Sensitivities to common foods can lead to leaky gut syndrome, promoting systemic inflammation and affecting blood glucose control.
Connection of Cortisol and Adrenal Health to Inflammation
Adrenal health is closely tied to blood sugar levels. Elevated cortisol from chronic stress can increase blood sugar independently of diet. Managing stress with practices like meditation and adequate rest is essential for long-term blood sugar control.
Final Thoughts on Blood Sugar and Inflammation Management
Understanding and addressing blood sugar imbalance is foundational in managing chronic inflammation and autoimmune disorders. Blood sugar stabilization provides a solid groundwork upon which other interventions, such as detoxification and infection management, can be more effective.By focusing on balanced nutrition, consistent physical activity, and stress management, individuals can take control of their blood sugar levels, significantly impacting overall health, mood, and inflammation levels. Managing blood sugar is one of the most effective steps to reducing chronic inflammation and supporting autoimmune health.
Want Personalized Support with Blood Sugar Imbalance (and Other Chronic Conditions)?
We offer Zoom consultations to help you identify the root cause. We order functional medicine lab tests for you and design a customized eating plan, supplementation plan and detoxification plan to optimize health while reducing the dependency on medications.
If you’re struggling with chronic symptoms, and looking for root cause approach using a natural and holistic approach, please visit https://askdrkan.com/get-started for more information and to get started on the path to wellness.